Frequently Asked Questions (FAQs)
Disclaimer:
The information provided in this Frequently Asked Questions (FAQ) section reflects the opinions and general guidance of The Circumcision Clinic. It is intended for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. We strongly recommend consultation with one of our healthcare professionals to address your specific concerns and receive personalized care. Every individual’s medical needs are unique, and only a thorough evaluation can provide the most accurate and tailored recommendations.
How The Circumcision Clinic is structured:
The Circumcision Clinic™ (The Clinic) coordinates high volume circumcision clinics at several locations across Ontario.
We bring expert, high volume, circumcision doctors to areas where there is underserved or unmet demand. The more demand, the more frequently we run our clinics.
We lease or rent space within clean, well-run medical clinics in these local geographies, where we set up our own doctors, administrative, nursing and support staff for the day.
As an example, ‘The Circumcision Clinic’ rents space within ‘BloorKids Pediatric Clinic’ (a wonderful, clean, bright and well-run general and specialist pediatric clinic!). When you set off for your appointment you can look for ‘BloorKids’ on your GPS. When you enter, you will see a sign and kiosk with ‘The Circumcision Clinic’ where ‘The Circumcision Clinic’ admin will check you in and guide you on the start of your journey. You will not interface with any personnel from ‘BloorKids’ despite this being the host for the appointment. (Though you are welcome and invited to speak to the ‘BloorKids’ reception about finding a pediatrician or specialist for your child while you are there.)
If you require any post-procedure follow-up, our team can help you to book your appointment virtually, or at any of our locations based on urgency and availability. (i.e., just because you visited the ‘BloorKids’ location for the original appointment, doesn’t mean you need to return to that location for follow-up care necessarily – though you can if you choose.)
The Clinic is founded on the idea that doctors and teams that do a high volume of procedures have better outcomes than practitioners that practice circumcision care on an ad hoc or infrequent basis.
The doctors and nurses work on a shared care model, so when you sign up for an appointment with The Circumcision Clinic™ you agree to the care of any of our wonderful doctors and nurses.
The Circumcision Clinic leadership will only support doctors who have a proven track record of excellent surgical outcomes AND excellent bedside manner and family-focused approach.
The Clinic doctors and nurses have standardized and established protocols for all the aspects of care where we have been able, ensuring a consistent experience across practitioners and locations.
Elements of care that are standardized amongst all doctors and locations were developed by consensus and approved by all physicians providing care. These include:
Consent forms and information for patients
Choice of, and route of, local anesthetic nerve block
Aftercare instructions
The doctor providing the circumcision takes on the full responsibility for the care they provide, so there might be differences between doctors with regard to inclusion criteria (safe age they will provide circumcision), technical approach to the procedure (tools, equipment and time to complete the surgery), or inclusion / exclusion of patients with minor anatomical variations (minor webbing or rotation etc.)
Note: if there is an anatomical variation that makes a clinic-based circumcision unsafe, The Circumcision Clinic™ will coordinate a referral with a specialist that can help you manage in a safer manner.
If you arrive for a circumcision appointment and after discussion with the team either you or your doctor decide it’s not best to move ahead with the procedure, there will be no charge for the visit. We do not want there to be any financial pressure on families to move ahead with the procedure.
What to Expect During Your Visit:
You should expect to be in the clinic for 1-1.5 hours.
The time spent in the clinic is typically broken down as follows:
Informed consent discussion (5-10 min)
Nerve block injection (5 min)
Time for the nerve block injection to be fully effective / time to feed the baby (10-20 min)
Circumcision procedure (10-15 min)
Teaching how to complete diaper changes and aftercare following the procedure (5 min)
Discharge home from clinic
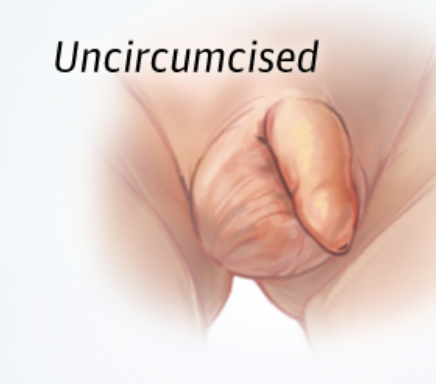
What is circumcision?
Circumcision is a procedure in which the foreskin (fold of skin that covers the end of the penis) is surgically removed.
Why do people choose to have their child circumcised?
• A decision to circumcise or not to circumcise a newborn son is a personal choice.
• Most newborn circumcisions are done for prevention of urinary tract infections, sexually transmitted diseases, and skin problems unique to the foreskin
• As well as traditional, cultural, or religious reasons.
• Custom / Culture / Religion
• Circumcision of the male infant is commonly done by custom. Many parents feel it is important that their son looks like his father or peers or have a religious obligation to have their son circumcised.
• Cleanliness
• Circumcision makes cleaning the penis easier. A normal secretion, which is cream-coloured and somewhat waxy, is formed under the intact foreskin. Circumcision prevents this buildup, but the buildup can also be prevented by proper hygiene during bathing. Circumcision does not eliminate the need for proper hygiene, though it makes it easier.
• Prevention of cancer of the penis
• Penile cancer is an extremely rare condition of adult life. It is less common in circumcised men and is usually found only in conditions of very poor hygiene, suggesting that proper hygiene provides as much protection as circumcision.
• Decreased incidence of infection
• Circumcision will slightly reduce the risk of urinary tract infections in males, both as infants and in adulthood. The incidence of such infections in the first year of life is reduced from 1 in 100 to 1 in 1,000. Circumcision has also been shown to be associated with a lower risk for some sexually transmitted infections, including HIV, particularly in areas where the use of safe sexual practices is low.
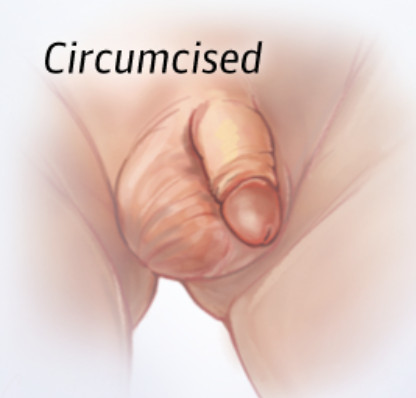
• Prevention of paraphimosis
• Rarely, parents may retract a still-tight foreskin while vigorously cleansing the penis to eliminate the waxy secretion mentioned above. If the foreskin is left retracted, it can act as a tourniquet, decreasing blood supply to the tip of the penis. This may need to be surgically corrected. Circumcision prevents this uncommon complication from occurring.
REASONS TO CHOOSE NOT TO HAVE A CIRCUMCISION
Pain
Although the maximum pain-relieving actions will be taken for your baby's comfort on the day of the procedure, there will be some degree of discomfort during the visit and through the first few days of recovery.
Surgical risk
The vast majority of circumcisions are performed without any complications. However, no surgical procedure (and circumcision is a surgical procedure) can be totally risk-free. Complications include: bleeding, infection, adhesion formation, cosmetic deformity, trauma to the penis, excessive removal of the foreskin, and functional defects. These occur once every 500 circumcisions.
Expense
Routine newborn circumcision is not covered by OHIP and therefore there is a cost attached to the procedure. Although parents have the option of delaying circumcision until a time beyond the newborn period, these delayed circumcisions represent a more involved surgical procedure, usually performed with general or regional anesthesia. It is important to note that 1 in 100 uncircumcised adults may require a circumcision for medical reasons.
Surgical risk in detail:
Minor short-term problems:
Slight oozing or slight bleeding (normal and expected)
Bruising and swelling
Superficial infection of the circumcision site or at the tip of the penis
Irritation of the exposed tip of the penis (glans)
Minor long-term problems:
The urethra, which leads from the bladder to the tip of the penis, can be damaged at its point of exit
The newly exposed meatus (urethral opening) can become stenotic (small) due to chronic irritation now that it is exposed to the diaper
Inappropriate scarring
Unintended removal of excessive skin layer (or layers) of the penis
Unintended removal of too little skin, leaving some redundant foreskin behind
Asymmetry to the cut line
The site of foreskin removal can scar, leaving an opening too small for the skin to retract over the penis (post circumcision phimosis)
Major problems that are very uncommon:
Complete removal of the skin covering the shaft of the penis
Significant, life threatening, bleeding, requiring stitches or other measure to stop the bleeding. Fluid administration or blood transfusion are needed in cases of severe blood loss
Serious, life-threatening bacterial infection
Partial or full removal (amputation) of the tip of the penis
There are different techniques for performing newborn circumcision. Is it important what technique is used? What is the difference from one technique vs another?
There are several ways that doctors can perform a newborn circumcision, they are typically described by the specific tools that are used. The techniques that our parents tend ask about include the use of either a Gomco, or a Mogen clamp, or use of a Plastibell ring. These three techniques are the most commonly used techniques for elective bedside newborn circumcision in North America.
If performed appropriately, by an experienced medical practitioner, all of these techniques should result in the same outcome. That is to say, once the circumcision wound is fully healed, there is no difference in how the penis looks whether the child was circumcised with a particular clamp or a ring.
Some circumcision clinics or circumcision doctors will promote one technique as being quicker, safer or providing a better cosmetic result. It is the opinion of The Circumcision Clinic that this is a marketing tactic and not necessarily the truth, nor the most important considerations when choosing a surgical technique.
Based on the experience of our clinical team, we believe most physicians practice using the technique in which they were trained in, or the technique that they gained the most experience with. Their choice of a specific tool is typically less informed by the specifications of the tool, and more informed by their comfort using the tool safely and effectively in their own hands - and we think this is the correct way to decide! We believe that is more important for doctors use the tools and techniques they are the most proficient with. The ‘better’ tool in less experienced hands if more likely to result in a complication than a ‘worse’ tool use by an experienced and competent provider.
There are reports of various complications with all the different techniques used for newborn circumcision. The medical literature consistently reports that complication rates are lowest with experienced providers.
Most of our doctors use a Mogen clamp; this is not something The Circumcision Clinic has mandated. It just so happens that this is the tool that our current doctors have used throughout their career and are very good with. The Clinic would be happy to support a doctor using another technique if they had a proven track record of excellence with that technique, as well as the same track record of excellence in bedside manner and commitment to post-procedure care.
As important as meticulous surgical technique, we believe the bundle of care, which includes pain control, thorough parent education about aftercare, and appropriate and expedient access to follow up is what leads to excellent outcomes.
Do parents ever arrive at the clinic, and then decide not to move forward with a circumcision procedure? Why does this happen? What do I need to know about this scenario?
If you arrive for a circumcision appointment and after discussion with the team either you or your doctor decide it’s not best to move ahead with the procedure, there will be no charge for the visit.
• We do not want there to be any financial pressure of families to move ahead with the procedure.
• Some common scenarios not to move forward with a circumcision even after arriving in the clinic:
• Some families arrive thinking that it is medically necessary for them to circumcise their child, and we dispel that idea.
• After learning more about the risks or the healing process, some families will change their mind.
• Sometimes parents just need a bit more time, especially if there is one partner who is not sure about the choice of circumcision.
• We encounter an anatomical contraindication to a clinic-based circumcision.
TO EXPAND ON THE POINTS ABOVE:
• Some families arrive thinking that it is medically necessary for them to circumcise their child, and we dispel that idea.
• Elective newborn circumcision is a choice based on the personal assessment of risks and benefits after thoughtful deliberation by the parents.
• Our team will never convince a parent that a circumcision is a better choice than not circumcising.
• The major pediatric and urologic societies tend to describe routine circumcision as not necessarily having a clear benefit.
• A circumcision cannot be reversed.
• If your child develops a medical indication for circumcision later in life the cost of the procedure is covered by the Ontario Health Insurance Plan (OHIP).
• After learning more about the risks or the healing process, families will change their mind.
• A major complication, though rare, can be devastating for the child or the family – and parents need to go into the procedure knowing that, though extremely rare, there can be bad outcomes (even with clinics and doctors that have great reputations).
• Sometimes parents need a bit more time, especially if there is one partner who is not sure about the choice of circumcision.
• We will never try convincing you that a child needs to be circumcised, but we are happy to explain all the ways that we mitigate pain and risk. One way we help is by offering quick access to follow-up (we remain available for any questions at any age after the procedure).
• Note: for families that know they want to have their child circumcised, we strongly believe that a newborn circumcision is the best approach and timeframe.
• We have found that the baby / family experience is best if children are less than 2 months old at the time of the procedure.
Can parents or family be with their baby during the procedure?
YES!
The clinic is designed to minimize the time your baby is out of your care. Parents and anyone that the parents have brought with them to the clinic are welcome to be with their child for all aspects of the care they receive.
Do I have to be in the room when my child undergoes the procedure?
NO!
We have staffing to help care for your child, so for parents that are uncomfortable watching the procedure, they do not need to be in the room. We do not rely on parents to hold or restrain their children.
What are some anatomical contraindication (issues with the way the penis has developed that prevent the doctors from offering a procedure) to a clinic-based circumcision?
There are several anatomical variations where it is unsafe or ill-advised to move forward with a circumcision without a pediatric urologist consultation. These include:
Severe Hypospadias (meatus outside of the glans, ‘pee hole not on the head’)
Severe rotation
Severe webbing
Chordee
Bilateral undescended testicles in the absence of a karyotype.
Very small or very large penis.
Buried penis
WE HAVE SOME MORE DETAILS ABOUT THESE ANATOMICAL VARIATIONS BELOW
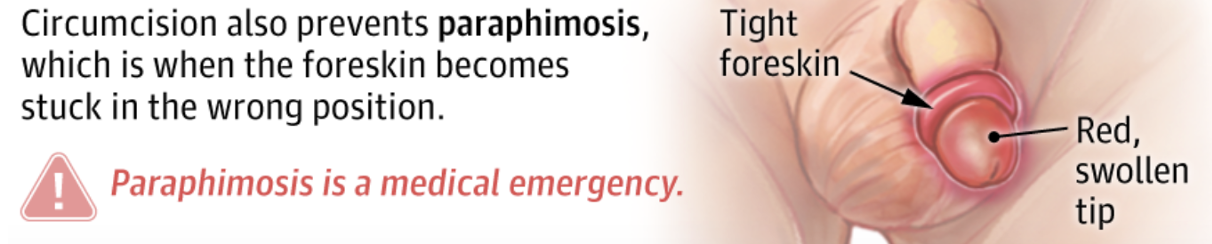
What is HYPOSPADIAS and can I still have my son circumcised if they have a HYPOSPADIAS?
Hypospadias is a congenital condition in which the opening of the urethra, called a meatus (pee hole), is on the underside of the penis rather than at the very tip.
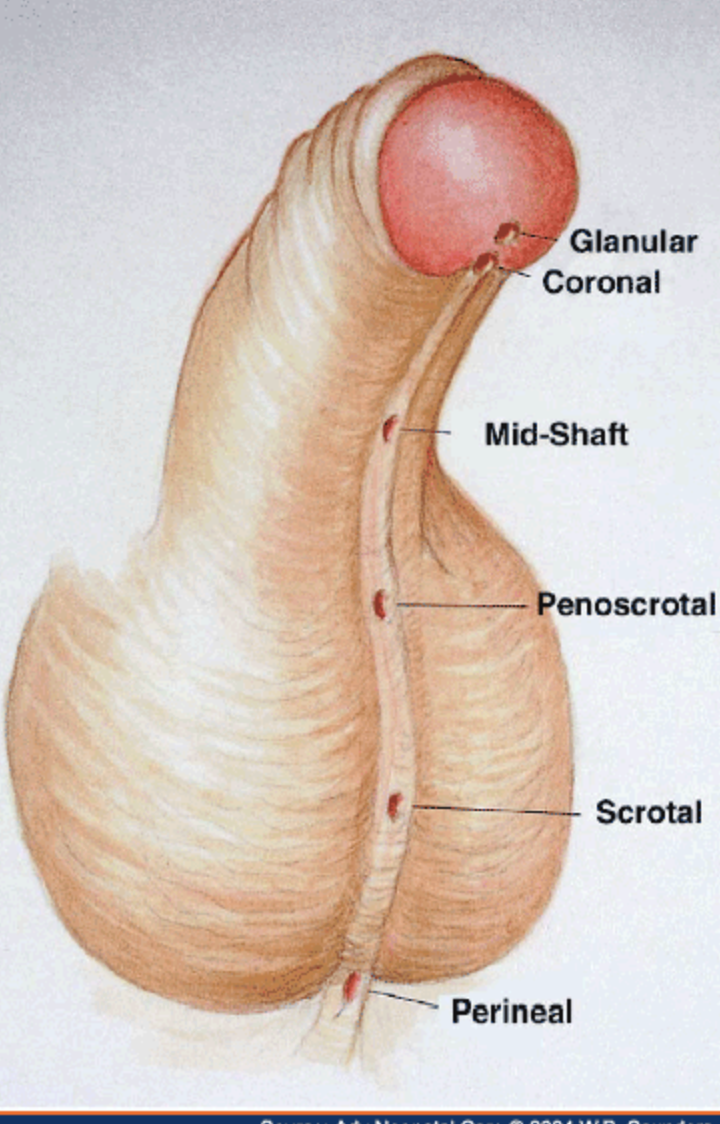
The condition is classified by the location of the meatus (pee hole):
Distal (anterior): The opening is located near the head of the penis. This is the most common and mildest form.
Midshaft: The opening is located along the middle of the penis shaft.
Proximal (posterior): The opening is at the base of the penis, in the scrotum, or behind the scrotum. This is the most severe and least common form.
Hypospadias is present at birth, it occurs in approximately 1 in 200 male infants.
If the pee hole exits on the margin of the head and the shaft skin, or below, we cannot perform a circumcision in our clinic and children need to be seen by a pediatric urologist for a corrective procedure (which can include a circumcision at that time).
For milder forms of hypospadias, where the meatus clearly exits on the glans we can offer a circumcision in our clinic. The mildest form of a hypospadias with a hooded foreskin, where the foreskin is incomplete on the underside, but the meatus (pee hole) is in the correct position at the tip of the glans (head). The circumcision in the clinic will not change the location of the pee hole, and when boy grow that will have to adjust how they aim to compensate. Some families are happy to move forward with a circumcision knowing this. Some families prefer to see a pediatric urologist for a more comprehensive discussion about what is required to move the pee hole if necessary.
FOR FAMILIES OF BOYS WITH MILD HYPOSPADIAS (PEE HOLE EXITS WITHIN THE HEAD) OR A HOODED FORESKIN WHO KNOW THEY DO NOT WANT TO SEE A PEDIATRIC UROLOGIST OR HAVE ALREADY SEEN A PEDIATRIC UROLOGIST WHO HAS COUNSELLED FAMILIES THAT A MOVE COMPLICATED REPAIR IS UNNECESSARY, WE ARE ABLE TO OFFER CIRCUMCISION IN THE CLINIC.
What is a WEBBED PENIS or PENOSCROTAL WEBBING, and can I still have my son circumcised if they have this?
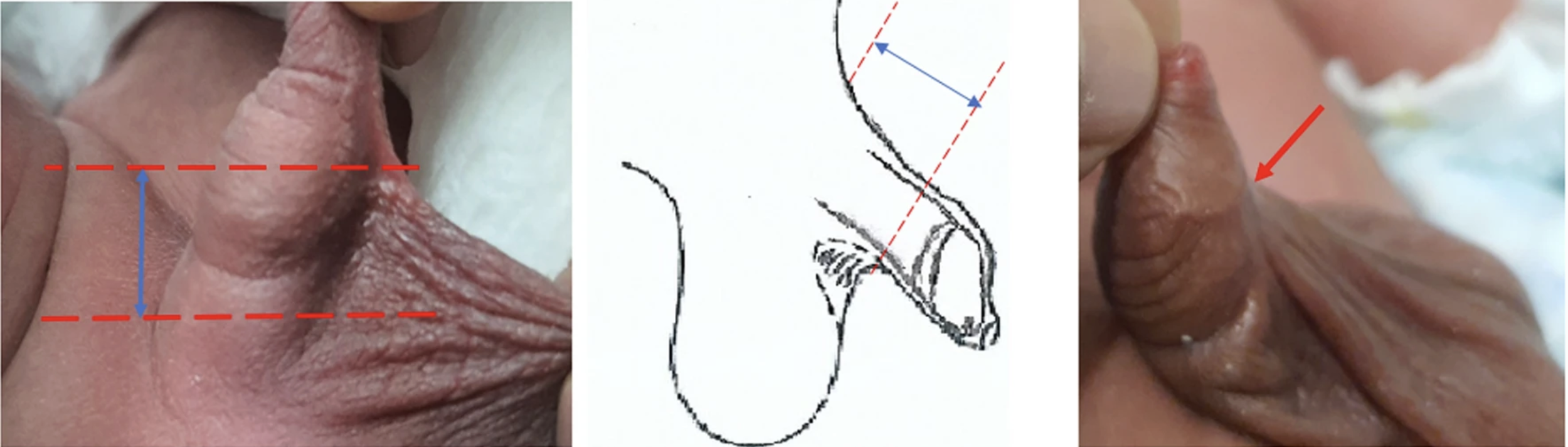
A webbed penis, also known as penoscrotal webbing, is a where the skin of the scrotum extends abnormally high onto the underside (ventral shaft) of the penis. This creates a fold or "web" of skin between the penis and the scrotum, which some people describe as a "turkey neck" appearance.
The severity of webbed penis (penoscrotal webbing) exists on a spectrum from mild to severe based on how far the scrotal skin extends up the ventral (underside) penile shaft. The more extensive the webbing, the more severe the condition.
For milder forms of webbing, where there is some ventral skin (skin on the underside) still preserved, we can offer a circumcision in our clinic. We make some minor adjustments to the angle of the cut, to preserve the skin on the underside of the penis. This surgical modification is something that neither the parents nor the patient will notice, as the result is a simply a normal appearing penis, as though there was no webbing to begin with. The doctors at The Circumcision Clinic have extensive experience with this form of minor anatomical variation.
In more severe cases, it is preferential for a pediatric urologist to perform the circumcision, as more advanced surgical techniques are required.
As mentioned, penoscrotal webbing exists on a continuum, and the choice to move forward in the office with The Circumcision Clinic, versus with a pediatric urologist is something that should be decided with a full understanding of the risks and benefits. If the doctor at the circumcision clinic does not feel confident that they can provide a good outcome based on the anatomy, they will help coordinate a referral to a pediatric urologist for ongoing management.
Some parents ask, ‘wouldn’t it be better to have all variations of a webbed penis treated by a specialist in an operating room?’. Firstly, there is good medical evidence to suggest that for appropriately selected anatomy (1,2), the outcomes with an office-based procedure are just as good as a more extensive surgery in an operating room. Since the procedure is less extensive, recovery is quicker, offering an advantage. Furthermore, there are practical considerations that we believe makes the clinic setting preferential. Firstly, an operating room-based procedure often requires a general anesthetic, which poses its own set of risks. Secondly, most pediatric urologist won’t offer the procedure until children are older to mitigate both the anesthetic risk, and to give time for the anatomy to grow. Thirdly, in Ontario there are waitlist and backlogs for elective circumcision, so the wait for an operating room-based procedure can extend for several years. Finally, once you require an operating room setting for the procedure, the cost increases, often exceeding thousands of dollars.
FOR FAMILIES OF BOYS WITH MILD OR MODERATE WEBBING, WHERE THERE IS SOME VENTRAL SKIN (SKIN ON THE UNDERSIDE) STILL PRESERVED, WHO KNOW THEY DO NOT WANT TO SEE A PEDIATRIC UROLOGIST OR HAVE ALREADY SEEN A PEDIATRIC UROLOGIST WHO HAS COUNSELLED FAMILIES THAT A MOVE COMPLICATED REPAIR IS UNNECESSARY, WE ARE ABLE TO OFFER CIRCUMCISION IN THE CLINIC.
Bawazir, O.A., Alhallaq, O.A., Albayhani, B. et al. Is the simple webbed penis a contraindication to circumcision?. Afr J Urol 27, 132 (2021). https://doi.org/10.1186/s12301-021-00235-w
Maizels M, Meade P, Rosoklija I, Mitchell M, Liu D. Outcome of circumcision for newborns with penoscrotal web: oblique skin incision followed by penis shaft skin physical therapy shows success. J Pediatr Urol. 2019 Aug;15(4):404.e1-404.e8. doi: 10.1016/j.jpurol.2019.05.021. Epub 2019 May 27. PMID: 31337533.
What is the best age to have a newborn circumcision?
We have found that the baby / family experience is best if children are less than 2 months old at the time of the procedure.
The younger the better.
It is safe to perform a circumcision on the day after delivery if the child is healthy.
WHY IS YOUNGER BETTER?
Stronger calming from sucrose taste
Less skin means less bleeding
More comfortable lying flay on the back for a few minutes during the procedure.
Younger babies tend to feed and sleep more during recovery, with less signs of discomfort (less crying and fussing) during the 2-3 days that the wound is sore after the procedure.
Most clinics only offer circumcisions for children less than 6-8 weeks old. WHAT CHANGES AS CHILDREN GET OLDER IN TERMS OF THE PROCEDURE AND RECOVERY?
We have an extensive experience offering circumcision for children up until 6 months old. It is described in the medical literature that complications such as bleeding or infection rates are higher for children outside of the newborn period. Our clinic has not had any issue with the surgery or the recovery for our older patients.
THE IMPORTANT INFORMATION PARENTS NEED TO APPRECIATE IF THEIR CHILD IS OLDER THAN 8 WEEKS:
Younger newborns (8 weeks or less) tend to have a stronger reflex to relax in response to tasting sucrose. As they get older, this no longer works the same way and therefore, as soon as we lie the children flat, and use Velcro straps to restrain the legs, they tend to fuss and try to sit up.
Despite the nerve block injection, older babies tend to cry throughout the procedure simply from the positioning.
We perform the procedure despite this fussing and accept they will cry and wriggle around throughout.
The surgical technique is designed to work even when babies are wriggling or moving, so there is not a risk that the movement will lead to a surgical error (this is an understandable fear or concern from many of our families). However, the wriggling and movement is challenging for the parents to watch and witness.
At our clinics, we allow parents to be with their children for all element of the procedure. This means, for parents who choose, they can be in the procedure room. For older children, seeing their child restrained and crying can be difficult to witness and distressing. This should be carefully considered before deciding whether to be present or not.
We are often asked how we can be sure the crying is from the positioning, rather than from pain – perhaps the nerve block is not working fully or as intended. The truth is, if babies start crying during positioning and wont settle, it is challenging to know for sure what they are feeling. Typically, the crying doesn’t worsen from the parts of the procedure that we know would be painful, and we see that children settle very quickly once the procedure is over and they are back in their parents arms.
Also, we occasionally have older children that don’t fuss from the positioning, and in these cases, we don’t see a reaction to the surgery that would indicate pain. From these children we gain confidence that the nerve block is effective – even for children who are fussing from the get go.
So we assume that children who are fussing from the moment we get them in position for the procedure are not experiencing the pain of the procedure.
When we agree to perform the procedure for older children, we enter into an agreement with the parents that they are OK with this the procedure to take place while the child is visibly upset.
What to know about the local anesthetic nerve block injection and pain control during the procedure.
Pain control for the circumcision is achieved by injecting a small amount of local anesthetic (usually 1mL of 0.25% Bupivacaine with 1:200,000 epinephrine) in the area where the nerves are located that provided sensation to the end of the penis and the foreskin (dorsal penile ring nerve block).
Injection is done with an extremely thin 27-gauge needle.
Needle insertion causes minimal pain; however, the medication stings as it enters the body.
The best analogy for most parents is that the feeling is like the injection that dentists use in the gums prior to a dental procedure
To maximize the baby’s comfort during the injection, sucrose (sugar water) is given on a pacifier or gloved finger with therapeutic suck to help soothe the baby.
Bupivacaine is a long-acting local anesthetic and theoretically there should be complete block of any pain sensation for the first 3-6 hours after injection.
The local anesthetic doesn’t turn off at the 3-6 hour mark. The effects slowly fade away for up to 12 hours, meaning there is some degree of decreased pain for 12-18 hours after injection.
It is normal to see swelling or fullness in the area around the injection sites where the local anesthetic is infiltrated / injected underneath the skin.
It is normal to see some evidence of bleeding or bruising at the injection sites that will resolve as the circumcision wound heals – over the course of 1 – 2 weeks.
It is normal to see blanching (pale colour) in the area around the injection sites (this is from the epinephrine causing slightly reduced blood flow in the area).
The local anesthetic come pre-mixed with a low concentration of epinephrine. The addition of epinephrine helps in several ways.
It causes constriction of the small capillaries in the area where the medication is deposited. This means the medication is not cleared away from this area by the blood flow as quickly, increasing the duration of the block.
Because the medication is not cleared away in the blood stream as quickly, it lowers the chance of spiking high concentration of local anesthetic in the blood, thereby lowering the chance of a systemic toxicity.
The capillary constriction reduces the amount of bleeding during and after the procedure.
Below is a video of one of our doctors administering the dorsal penile nerve injection while talking through his approach to the technique.
Dorsal Penile Nerve Block Prior To Newborn Circumcision
How do you perform a newborn circumcision in the clinic?
All of the the doctors at the Circumcision use a tool called a Mogen Clamp to perform the circumcision procedure. Below is a description of the surgical technique, followed by a video of one of our doctors performing the procedure.
Once 10-15 minutes had passed following the dorsal penile nerve block injection (after the block has had an appropriate time to have the full effect) the child returns to the procedure room for the circumcision. The foreskin, shaft, and base of penis are prepped with chlorhexidine (an alcohol used to disinfect the skin prior to the surgery). The surgeon puts on sterile surgical gloves and drapes the penis with a sterile drape. The foreskin is retracted, and the mucosa (inner foreskin which is often stuck or adherent against the head) is separated from the glans (head) using sterile gauze and a blunt dissecting probe. The foreskin is returned to neutral position before the incision line is measured and marked with a sterile skin marker. A mosquito snap (surgical tool) is placed on the dorsal aspect (top) of the foreskin before a Mogen clamp is applied. Prior to closing the clamp, the site is carefully inspected to ensure that the appropriate amount of foreskin is going to be removed, and that the glans (head of the penis) is safely below the clamp (rather than trapped in the opening). The clamp is closed, protecting the head from injury and ensuring a cut that aligns with the markings, even if the child is wriggling or moving in the restraints. A scalpel blade is used to cut away the foreskin above the clamp. The clamp is then opened, at which point the shaft skin edges are press-sealed in front of the head. At this point the head is concealed momentarily, before the shaft is gently pulled down, which allows the head to come out, revealing the final result.
Below is a video of one of our doctors performing a newborn circumcision in our clinic:
A video of one of our doctors performing a newborn circumcision in our clinic
Why not use a topical anesthetic ointment or cream (EMLA) instead of a nerve block:
Some doctors perform circumcision after application of a topical anesthetic cream (such as EMLA) instead of an injectable nerve block.
Creams are only partially affective at reducing the sensation of the circumcision and cannot achieve a complete block.
The duration of action of the cream is much shorter than the injectable medication.
An injection offers a total block of any pain sensation during and after the procedure for several hours.
Why not use a topical anesthetic ointment or cream (EMLA) before the nerve block:
When the clinic first opened, we went through a period of time when we instructed parents to apply a topical anesthetic cream (such as EMLA) over the area where the needle would enter the skin for the nerve block injection. The idea was that we could further improve the pain experience by numbing the skins sensation of the needle entry and injection.
We found that despite the application of the anesthetic cream, the injection would cause a pain reaction during the injection of the local anesthetic deep to the skin, in the layer that is not reached by the topical cream.
The needle that we use to inject the local anesthetic is very thin, similar to an acupuncture needle. Even without the use of a topical anesthetic cream, we don’t see a significant reaction to the needle passing through the skin in most of our patients. In fact, many patients don’t react at all to the needle entering the skin (in part because we give sucrose by mouth prior to injection).
Based on these consistent observations, we decided that the application of the cream is not improving the pain experience. Furthermore, even topical creams are absorbed into the bloodstream and can theoretically result in adverse medication reactions.
We decided that, on balance, the risks of asking our families to apply a topical cream (theoretical reaction to the medication in the creams), outweighed the benefit (minimal- to no-reduction in the pain response).
As such, we have since stopped recommending that parents apply an anesthetic cream prior to arrival.
How do you know the nerve block is working before you start the procedure?
Before we begin the procedure, we test by pinching a small area of the foreskin.
If the baby reacts to this pinch, this is evidence of inadequate block we inject more local anesthetic and wait.
Sometimes we witness discomfort and suspect it may be from other reasons. Babies don’t like the experience of lying flat on their backs, they may be gassy, hungry or tired.
We gauge whether fussiness is due to pain based on whether the crying is in keeping with the surgical manipulation, or independent.
Though pain sensation is blocked by the local anesthetic, pushing and pulling are still perceived and can also lead to the baby reacting.
Fussiness and movement will not interfere with the technical success of the procedure.
The procedure is designed to be safe even with relatively large movements by the baby.
We believe we are doing the maximum to improve the pain experience that can safely be achieved in a clinic setting.
Does the baby need to have received a Vitamin K injection to have a circumcision?
Vitamin K is crucial for blood clotting because it's a cofactor for enzymes that produce clotting factors, proteins essential for forming blood clots.
Without enough Vitamin K, the body can't make these proteins, leading to impaired blood clotting and potential bleeding problems.
Babies are born with low Vitamin K levels because it doesn't readily pass from mother to fetus during pregnancy.
In Canada, all newborns routinely receive a Vitamin K injection shortly after birth to prevent Vitamin K Deficiency Bleeding (VKDB).
VKDB is a rare but serious condition where a baby's blood cannot clot properly, potentially leading to severe bleeding in the brain and other organs. The injection is a standard preventative measure, given within the first six hours after birth, and is considered highly effective.
Some parents decline for the baby to receive the Vitamin K injection at birth. These children have a higher risk of post-circumcision bleeding (and other bleeding). This risk likely returns to normal somewhere between 8 weeks and 6 months of age.
When families have chosen not to give their child the vitamin K injection, The Circumcision Clinic will only offer a circumcision after 2 months of age.
Some families opt to give their child Vitimin K by mouth instead of by injection. This rout of administration is less reliable in increasing the clotting factors and we also will only offer a circumcision after 2 months of age.
Can a child with Jaundice have a newborn circumcision?
Jaundice in newborns is the yellow coloring in an infant’s skin. Jaundice occurs when bilirubin (pronounced “bil-ih-ROO-bin”) builds up in the baby’s blood. Hyperbilirubinemia is the medical term for this condition.
Bilirubin is a yellow substance the body creates when red blood cells break down as part of normal function. During pregnancy, the mothers liver removes the bilirubin. After birth, the baby’s liver must begin removing bilirubin. If the liver isn’t developed enough, it may not be able to get rid of bilirubin. When excess bilirubin builds up, the baby’s skin may appear yellow.
Jaundice in infants is common. It’s usually not serious and goes away within a couple of weeks. Severe jaundice can lead to brain damage if it goes untreated. It’s important for the baby’s healthcare provider to check jaundice levels and treat if it is severe.
50–80% of term newborns develop jaundice, or hyperbilirubinemia (HB), in their first week.
The vast majority have benign causes, including physiologic jaundice of the newborn and breast milk/breastfeeding jaundice, which do not affect the livers ability to make clotting factors.
Though uncommon, HB in the setting of sepsis, biliary obstruction, or metabolic disease, may increase bleeding risk. These babies typically show signs that they are sick, beyond the jaundice itself (fever, poor feeding, lethargy)
A review of the scientific literature suggests that isolated HB in otherwise healthy newborns does not increase bleeding risk.
Review of the scientific literature suggests that in otherwise healthy neonates, jaundice likely represents benign causes and is unlikely to increase bleeding risk
At The Circumcision Clinic we are happy to offer circumcision procedures to children with mild jaundice who are otherwise healthy.
https://www.sciencedirect.com/science/article/abs/pii/S1477513120305659
What is ‘sucrose’ and why do you give sucrose to the babies during the local anesthetic injection and during the procedure?
Sucrose is the chemical name for table sugar.
The use of sucrose is established and used routinely in pediatric hospitals due to a well researched reflex where newborn relax upon tasting.
Many parents might have seen sucrose used to help calm their newborns during the heel-prick blood draw or vitamin K injection shortly after birth.
The concentration we use is shown in the medical literature to maximize the baby’s comfort during procedures (24% sucrose in water).
We apply the sucrose on a pacifier or gloved finger before and during injection and again during the actual circumcision procedure.
There is more to calming babies than the taste of sucrose alone – the staff that give the sucrose have a special skill for calming the babies with gentle touch, shushing and soothing. The entire package is what helps keep babies calm. This is a skill gained through experience.
Even though the penis is completely numbed from the nerve block injection prior to starting the circumcision procedure, we give sucrose to help babies feel relaxed while their legs are gently restrained with Velcro straps, and they are lying flat on their backs.
It is the taste of the sucrose that leads to the reflex to relax. Therefore, we are not feeding the sucrose like you would feed milk. We use a dropper to flavour the pacifier or gloved finger and only use 1-5mL throughout the entire clinic visit.
This is not enough sugar to impact blood sugar or metabolism in a harmful way.
What to expect immediately following the procedure:
If the parents are not already in the room during the procedure, we bring them in immediately afterwards to have a close look at the results of the circumcision.
It is important for parents to see the results of the procedure so they can better appreciate how it will evolve during the healing, and to see that there were no surgical complications.
Note: In the rare event of a surgical complication, parent are still brought in so they can be shown anything that is abnormal and discuss next steps in management.
Parents can expect to find their child lying on their backs with their legs gently strapped to a specially designed board.
An assistant will be using a gloved finger or a pacifier to sooth the baby.
Most babies, especially those less than two months old at the time of the procedure, will be calm and not showing any discomfort when parents are brought into the room.
Babies older than 2 months are typically much more active and don’t respond the same way to the sucrose sedation. Parents can expect them to be fussy throughout all elements of the circumcision process – even when the nerve block is working perfectly.
Some babies will be fussy, either due to some discomfort from being restrained, maybe they are gassy and uncomfortable on their backs (we never know for sure). In cases where the baby is obviously uncomfortable, we will speed up the discussion of the anatomy and healing to get the child back into a comfortable position in the parents' arms.
Below is a video of a typical post-procedure interaction. The baby is calm and the doctor is explaining the important features of the wound, what normal and abnormal bleeding would look like, and teaching how to apply petroleum jelly in the diaper.
Below is a video of a typical post-procedure interaction. The baby is calm and the doctor is explaining the important features of the wound, what normal and abnormal bleeding would look like, and teaching how to apply petroleum jelly in the diaper.
How will the penis look immediately after the circumcision and during healing?
The doctors at The Circumcision Clinic all use a Mogen clamp to guide the incision. When the circular shaft skin is squeezed in the straight clamp, pinched skin results at the top (12 o’clock / dorsal) and underside (6 o’clock / ventral). Immediately after the surgery, these pinches are present. As the wounds heals, they disappear, resulting in the expected final cosmetic appearance.
The pinch at the underside (6 o’clock / ventral) is typically more pronounced. Sometimes the scar thickens at this point leading to an appearance like a small pimple. As children grow, this invariably softens, falls flat and becomes imperceptible by sexual maturity (puberty)
As the healing progresses, the wound will develop a scab.
Due to the mucosal nature of this skin, if present at all, the scab will be a whitish or light yellowish crust.
This scab will be mixing with urine / petroleum jelly and stool and can have a mucous like appearance, often confused with puss.
This crust / secretions will be adherent to the penis and will slough off on their own. It should not be removed with forceful wiping.
By two weeks, the incision line should be fully healed.
There can be different pigmentation of the shaft skin and mucosal collar, which is normal.
Immediately after the circumcision, the head and area underneath (mucosal skin) will be raw and red, there is minimal swelling at this point so parents will gain a sense of the final proportions.
The cut line is the transitional line between the mucosal skin, which will have a pink or red colour, and the shaft skin that you are used to seeing from before the circumcision.
Over the next few minutes and hours, the areas adjacent to the cut line (the mucosal skin and shaft shin) may get very swollen. The mucosal skin often appears as a doughnut sitting under the head.
Note, even after the wound has fully healed, there can be some fullness, or puffiness of the mucosal collar just below the head of the penis for months.
The head of the penis (glans) is typically slightly red. This is because the foreskin of newborns is adherent to the head. During the circumcision, the inner foreskin is peeled off of the head. In the act of separating the foreskin from the head, a thin layer of skin cells is stripped away, leading to some redness (similar to a skin exfoliation).
You may see sterile ink near the incision site—this is applied with a sterile marker and will disappear over time.
In cases where there is some early bleeding, or in older children, we may apply a skin glue (Dermabond or SkinAffix). The skin glue has a light purple hue. As the glue hardens, it can look like small dried flakes of plastic that will slough off into the diaper while the wound heals—do not pull off these flakes. See the section on skin glue for more information.
You may see small white- or cream-coloured speckles called smegma (normal dried skin that had been trapped behind the foreskin before it was removed). The smegma will slough off with time.
Our usual practice is to leave the penis naked in the diaper without a dressing / wrap or bandage. Approximately 1/20 babies will have some bleeding that requires a bandage to be applied. Having a bandage is the exception rather than the rule. Please see the section on the bandage for more information.
Over the next hours the wound swells, bleeds as it clots naturally. Therefore, it is normal and expected to see blood streaks on the surface of the diaper for the first few diapers as the cut is establishing a scab. Please see the section on bleeding for a more detailed explanation.
With newborn circumcision, the healing occurs by a process called ‘'primary or secondary intention’, whereby the body forms a clot, the clot transitions to a scab which eventually falls away leaving a thin scar.
Healing by ‘primary intention’ is when the cut edges stay in close contact during the healing, and there is typically minimal scabbing which often looks like mucous (rather than the crust most people think about when they think of a scab). This mucous appearance is because the scab is kept moist with petroleum jelly in the diaper.
Often, areas of the cut line separate by a few millimeters. This gap undergoes a healing process called ‘secondary intention’ where the body develops granulation tissue (which appears like a straw-coloured plaque) spanning the gap as new skin develops underneath. The most common area for the wound to separate and undergo healing by secondary intention is the underside.
Note: The healing process is different from older child or adult circumcision which requires the skin edges to be stitched or glued together.
We only perform suture-less circumcision and limit our practice to babies and children that are young enough for this approach. Usually, within 1-2 weeks the scab has resolved and the incision is fully healed.
Can you explain a bit more about how you use SKIN GLUE / TOPICAL SKIN ADHESIVE / GLUE STITCH?
For older children, or in cases where there is more bleeding immediately after the procedure than usual, we occasionally apply a surgical skin glue / topical skin adhesive.
This is a commonly used sterile medical glue often used in emergency departments or by outdoor enthusiasts instead of stitches.
The generic name for the skin glue is 2-octyl cyanoacrylate.
Brand names include Dermabond®, Skin Affix ® or GluStitch ®
It is a sterile, liquid, skin adhesive that holds wound edges together.
The film will usually remain in place for 5 to 10 days, then, naturally slough (fall) off.
It appears like small plastic flakes when it sloughs off (like superglue coming off off your fingers!)
Do not actively remove the dried glue as it can sometimes pull away the scab leading to some fresh bleeding. Allows the glue to naturally slough (fall) off.
If a skin glue was used for your child, the doctor will let you know so you can anticipate what is described above.
What to know about the DRESSING OR BANDAGE?
On occasion there is more bleeding than usual immediately after the procedure and we apply a dressing / bandage to contain the bleeding while the wound established a clot.
WE ONLY APPLY A DRESSING FOR ABOUT 5% OF PATIENTS – THE MAJORITY ARE LEFT NAKED IN THE DIAPER AFTER THE CIRCUMCISION.
I.e., Don’t be alarmed or surprised if there is not a bandage or dressing. Most babies do not have anything on the penis after the procedure.
The inner layer of the bandage is a sterile Vaseline-impregnated gauze, then overtop is an elastic bandage, followed by some tape.
This dressing helps to control any fresh bleeding as the wound clots in the first few minutes. The dressing is not essential to the wound healing and may fall off early (even as early as the first diaper change). If the dressing falls off, just continue to apply Vaseline to the penis and diaper as described below.
If the dressing has not fallen off on its own within three days of the circumcision, it should be gently removed.
Sometimes the clot and scab are integrated into the bandage such that the bandage wont slide off easily when it is time to be removed (3 days after the procedure).
Do not pull the bandage off with force. Rather, unwrap or slip off the bandage partially (whatever can be achieved), apply a thick application of Vaseline, and allow the Vaseline to continue to soften the attachment for another diaper change.
Repeat over as many diaper changes as necessary until the bandage slips off.
If the scab pulls off with the bandage, it can lead to some fresh spotting of blood.
This is normal and no cause for concern. This type of bleeding almost always clots off naturally and does not require re-application of a dressing.
If the bleeding is excessive at this point, please go directly to the nearest emergency department.
Spotting or fresh bleeding a few days after the circumcision does not alter the final cosmetic outcome and will clot and heal as though there was never an issue.
WHAT TO DO IN CASE OF BLEEDING?
SCENARIO – Blood streaking and/or blood diluted with urine and Vaseline in the diaper, but no blood flowing from the wound:
This is common and expected for the first 1-2 days after circumcision. This is a result of the wound undergoing the normal process of clotting and healing. There is no need for any medical attention.
SCENARIO – Moderate bleeding, more blood in the diaper than expected, but no blood flowing from the wound:
This is a relatively common and a challenge for parents and providers. Our approach is to ask patients to upload photos of the blood in the diaper which triggered the concern, and then to send a second photo of the diaper 1-2 hours later. Please also call the clinic to alert us. If the amount of blood is not excessive, and the rate of bleeding is slowing, then there is nothing extra to do. If the bleeding is significant and persistent it is important to have the wound evaluated and potentially treated. Treatment may include ongoing observation, skin glue, cautery, stitching, or compressive bandaging depending on the specific case.
If a physician from The Circumcision Clinic is available, they will ask you to return to the clinic to offer treatment. If someone from The Circumcision Clinic is not available, it is best to go to your nearest emergency department.
While we do our best to answer calls and check emails consistently on the days we perform procedures, and have almost always been available to guide families, we cannot guarantee timely response or availability to see you personally.
It is always best to err on the side of caution and report to the emergency department if you are concerned.
SCENARIO – Brisk active bleeding:
Brisk, active bleeding is an emergency, and you should report to your local emergency department. It may represent an underlying bleeding disorder, or an injured vessel that needs specific treatment including cautery, stitching or compressive bandaging. The risk of delayed treatment is life threatening blood loss.
Please reach out to The Circumcision Clinic to let us know what is happening. In these cases, someone from our team will try to contact the emergency department while you are on route to alert them of your scenario and immanent arrival.
WHAT TO DO IF THERE IS CONCERN ABOUT INFECTION?
Infection after routine circumcision is rare.
If there is a true infection it requires specialized treatment that can include surgical drainage, antibiotics as part of comprehensive care. Infection can present with increasing sensitivity and pain of the wound, puss, foul smell, and fever which typically begins a few days after the surgery. If you have a concern about infection, reach out to the clinic. If there is a shared concern for infection, the team will coordinate care with a specialist.
More commonly, as part of normal healing, the wound secretes a straw colour liquid. This, mixed with petroleum jelly, may look like puss. In the absence of other symptoms, this is normal and will resolve as the wound heals. Most of the time, when parents send photos with a concern about infection, it is in-fact normal secretions. The Circumcision Clinic will let you know if the photos look normal so you have peace of mind and can avoid unnecessary emergency care.
o When we respond to photos and questions about wound secretions, the medical team can comment on the appearance being typical and consistent with normal healing. However, it is impossible to completely rule out infection based on a photo. We may ask for ongoing photos over the next few days to track the evolution of the healing.
o Infection after circumcision is rare. At the point of writing, after providing care to thousands of patients, The Circumcision Clinic has yet to have a patient return with an infection. We do not attribute this to anything specific that the clinic is doing to limit infection ‘better’ than anyone else that offers circumcision. We use meticulous sterile technique during the procedure – and then immediately close the same diaper that the child was in at the start. This diaper is covered in the baby’s normal bacteria and this quickly covers the wound. The body and the skin have a robust system to protect from this bacteria. The circumcision wound is a skin incision and the infection rate is similar to the rate at which any small cut on the body develops an infection.
If you think about all the small scratches, cuts in the kitchen, cuts while shaving , skinned knees and elbows etc. that someone encounters in their life, developing an infection (abscess or collection of pus) is rare. This is the same with the circumcision wound. We describe this to inform parents just how rare infection is – and to help them feel comfortable when they face the inevitable scenario of stool that comes into contact with the wound. This doesn’t mean that there will not be an infection. But we believe that there is nothing more than usual diaper care and hand hygiene that parents need to do.
If we identify an infection that requires specific treatment, The Circumcision Clinic team will coordinate care with a pediatric urology specialist for ongoing management. The team will do everything necessary to ensure appropriate care is received as quickly as needed.
While we do our best to communicate consistently, and have almost always been available to guide families, we cannot guarantee timely response or availability to see you personally.
It is always best to err on the side of caution and report to the emergency department if you are concerned.
WHAT TO DO IF THERE IS CONCERN ABOUT THE HEALING OR COSMETIC OUTCOME?
While most cases heal without issue, up to 10% of cases will develop some degree of wound sticking, asymmetrical swelling, partial or complete re-covering of the head by the shaft skin (concealed appearance) as babies gain weight and grow. None of these problems are an emergency and will often self-resolve with growth and time.
•Wound sticking
In the case of wound sticking, a problem called a skin bridge (abnormal attachment of the wound to the head) can occur. It is relatively straightforward to release these attachments in the clinic with pain controlled with topical anesthetic cream or local injection. If you have concern of inappropriate wound sticking, you are welcome to contact our office. If intervention is required, you will be offered a follow-up appointment.
Persistent puffiness under the head, mild to moderate asymmetry, mild to moderate redundancy (partial foreskin left behind)
If there is persistent or asymmetrical swelling, or partial or complete covering of the head due to weight gain, this will almost always resolve over time and requires no extra intervention. Sometimes it is only during puberty that rapid growth leads to improvement in the cosmetic outcome. We are always happy to counsel parents and patients if there are concerns.
Significant asymmetry or redundancy
If the asymmetry or redundancy is significant, we coordinate referral to a pediatric urologist for consideration for a touch-up to revise the wound. This is rare.
Everything looked normal early on after the circumcision, now he is chubby and the head is completely covered by the shaft skin or fat nearby – is this normal? Is there anything special I should do?
It can be completely normal to see the shaft skin sliding over and covering the head.
When babies are chubby and carry their fat at the base of the penis, this pushes the shaft skin forward such that it may completely or partially cover the head. When your children grow, the fat redistributes, and the final cosmetic outcome will be as you might expect, with the head resting uncovered when flaccid. This may take years depending on how they gain and carry their weight. Sometimes it is only at puberty that the final cosmetic outcome matches the expectations.
Parents may be concerned that there is redundant or left over skin that was not completely removed. This is seldom the case. If you are worried about this, photos uploaded through our secure electronic portal within our electronic medical records, or an in-person exam can help differentiate the cause and inform ongoing care.
A few things that are normal and expected with babies when the shaft skin is covering the head:
1) The skin touching the head can adhere or stick to the head. Most of the time, these adhesions release spontaneously as the baby grows and there is no need to mechanically separate the adhesions. Similarly, there is no need for steroid creams to treat these. When parents are particularly concerned about the adhesions and want to see the head of the penis uncovered, we are happy to bring the child into the clinic and use a blunt probe and finger traction to pull apart the stuck skin. We typically ask parents to apply a topical anesthetic cream, such as EMLA, to minimize the discomfort that is related to this maneuver. Unsticking adhesions does not require cutting. When the skin layers pull apart the newly exposed skin can look raw and there can be a bit of spotting of fresh blood. The best analogy is like pulling a scab a few days before it is meant to release on its own. We perform this maneuver primarily to ease parental anxiety. – so they can get a view of the normal penis and see how easily the layers unstick. It is likely that the adhesions will re-occur and at that point we hope parents have a better understanding of the nature of the adhesions and can fully appreciate how this will self-resolve with growth, movement, spontaneous erections.
2) Dried skin cells and oils can collect underneath the skin. This is called smegma and appears as a white or cream coloured discharge. This does not represent an infection and should not be treated with medicated ointments or anti-fungal creams. This can be cleaned with soapy water at bath time. The best analogy for these collections is to think of them as similar to the lint that collects in the bellybutton. Though it may smell and appear concerning, regular bathing and hygiene is all that is needed.
3) If you are unable to easily slide the skin back to expose the head, this might represent a type of thick scarring called a post-circumcision phimosis. Thick scarring such that the skin doesn’t slide back and forth will benefit from treatment with low dose steroid creams to soften the scar and ensure appropriate sliding and growth. A post-circumcision phimosis commonly resolves with 6-12 weeks of twice daily treatments with low dose steroid creams (0.05% Betamethasone cream). In rare cases a minor surgical procedure is required to release the scar. In very rare cases, the scar can constrict to leave a very small opening in front of the head, creating an obstruction to urinary flow. If there is ballooning of the skin in front of the head when the child urinates, a very thin urinary stream, or a stream that sprays in multiple directions, this can require a more urgent stretching of the skin or surgical release of the scar – otherwise it can lead to kidney damage. A restriction or obstruction to the flow of urine caused by a post-circumcision phimosis should be treated as an emergency.
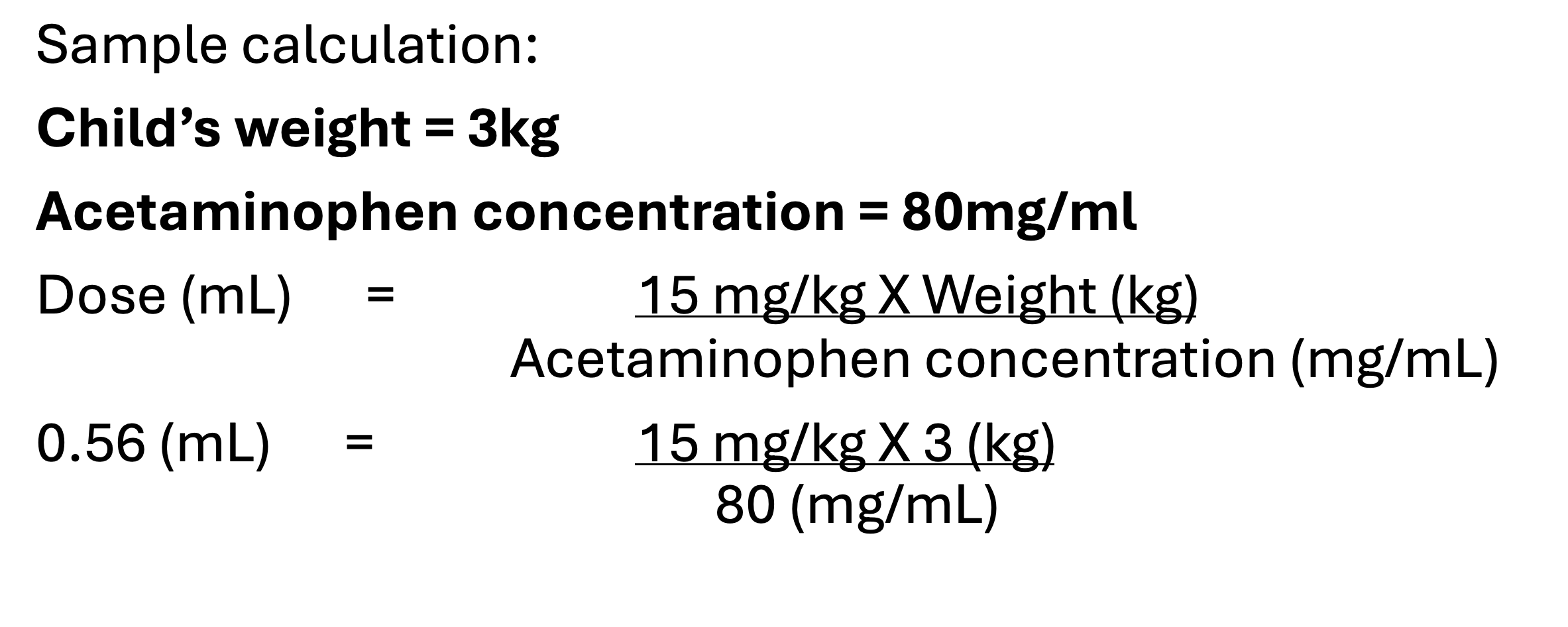
ACETAMINOPHEN (Tylenol® or Tempra®) for treatment of pain after the circumcision:
Acetaminophen is the generic medication name for Tylenol® or Tempra®.
Acetaminophen is a pain medication that can help babies feel better during recovery.
Some parents prefer not to use Acetaminophen during recovery - this is an acceptable option.
This medication can reduce pain, but will not completely eliminate pain during recovery. Therefore, it is still expected for children to be fussy and cry despite the use of this medication.
If Acetaminophen is given at the correct dose and at the correct frequency it is safe.
Dosing errors or overuse can cause harm.
Acetaminophen comes in liquid formulation at various concentrations, so it is important to check the bottle and do the correct calculations to dose the medication safely.
DO NOT GIVE A DOSE IF LESS THAN 6 HOURS HAS PASSED FROM THE PREVIOUS DOSE.
DO NOT CONTINUE TO USE AFTER 3 DAYS FROM THE PROCEDURE.
IF YOUR CHILD HAS A FEVER AFTER CIRCUMCISION, THEY NEED TO BE ASSESSED BY A PEDIATRICIAN URGENTLY
THE CIRCUMCISION WILL NOT CAUSE A FEVER.
What to know about CAR SEATS, CARRIERS, STROLLERS, AND HOLDING YOUR BABY:
There are no limits to how you should hold or move your baby.
Car seats, carriers, and strollers are all fine to use immediately.
If you sense that your baby is uncomfortable in a particular position, adjust as necessary.
Do not fear that these routine positions will impact the healing of the wound.
What to know about BATHING after the circumcision:
Sponge baths are suggested for the first three days after the circumcision.
During this time, the penis can be cleaned, if necessary, by squeezing warm water over it from a washcloth.
Immersion may take place beginning with the fourth day.
Drying should be accomplished by gentle patting.
Soaps are permitted.
What to know about URINATION following the circumcision:
Urine is normally sterile and will not cause any stinging or irritation. If there is no urine in the diaper in the first 12 hours after the circumcision, this is abnormal and you should be seen in the emergency department immediately.
Follow-up after circumcision
· Following a circumcision procedure in patients with normal or typical anatomy that proceed uneventfully (without complication) there is no scheduled follow-up.
· The clinic attempts to call every family on the day after the procedure to check-in and offer guidance for issues the family might be navigating.
· Most patients transition through the recovery uneventfully, and therefore, a visit with the clinic does not improve the outcome or change management.
· There are some situations where the clinic physician will plan a follow-up after a circumcision. These are usually in cases where there is something about the anatomy or the procedure that can lead to specific complications without early or ongoing assessment.
o This is most common situation where we pre-emptively organize follow-up is for babies that have an inconspicuous, concealed or hidden appearance (see separate section for more information) as these patients have a higher risk of developing adhesions (skin sticking) or post-circumcision phimosis (wound closing in front of the head) without specific aftercare which can include retractions or creams.
· The clinic aims to provide all the information parents need to navigate the recovery independently following the procedure. This is achieved through parent and care-giver education. Parent education includes:
o Materials available on this website.
o Materials sent through email at the time of the appointment booking and sent as reminders closer to the appointment date.
o Materials sent through the secure electronic medical record portal on the date of the circumcision.
o Informed consent discussion with the healthcare team during the appointment, prior to the procedure (this is an opportunity for parents to ask any questions before the procedure).
o Thorough overview of the wound and aftercare with the physician after the procedure
§ Following the procedure, if parents are not already in the procedure room to watch the surgery, parents are brought into the room to closely examine the circumcision wound and shown how to apply Vaseline with routine diaper care.
§ During this interaction, the evolution of the healing wound will be described, while specific parts of the anatomy are pointed out. The doctors will show you the incision line, the areas to expect swelling, bleeding and scabbing etc. This is all done to help parents understand normal healing.
§ It is during this interaction that we can reenforce:
· what to do in situations of normal vs excessive bleeding (superficial bleeding on the surface of the diaper is normal and expected for a few diaper changes as the cut clots and begins to form a scab. Blood soaking deep into the layers of the diaper, or thick clots in the diaper represent a dangerous amount of bleeding and children should be taken urgently to the closest emergency department).
· What to do during diapering, specifically when there is stool in contact with the penis
o wipe away gently with normal wet-wipes or warm water and a cloth – whatever is the normal routine can be maintained.
o Maintain a normal diapering routine, change the diaper when you would otherwise, when it is saturated with urine, or there is a pooh.
o Be a bit gentler when wiping the wound itself, as the wound is sensitive for up to 3 days.
§ NOTE: the wound CAN be touched lightly to clean.
o Try not to intentionally wipe away any clot or scab. This can re-open the wound and lead to some new bleeding.
§ If this happens, the bleeding will re-clot and the wound will move through the healing process again.
§ This might delay healing by a few days but does not cause any difference in the outcome. I.e., there won’t be more scarring or a higher rate of infection when this happens – so no need to worry.
· Crying is normal and expected.
o Acetaminophen (Tylenol) is an option and can be used to help ease the discomfort.
o That crying without a secondary symptom such as excessive bleeding does not indicate a further complication (this is a commonly asked question – ‘my child is crying, could this indicate some complication from the circumcision that needs to be fixed?’) Unfortunately, this is not a data point or information that can help point to a specific problem.
o Crying can be related to pain, or many other normal processes such as gas, hunger, tiredness etc.
· Despite the effort to provide as much information as necessary for parents to navigate recovery independently, it is common and understandable that parents remained concerned and worried about:
o The appearance of the healing wound.
o Changes in their child’s behaviour.
o What to do in the face of other parenting concerns, ie:
§ Can my child get a routine vaccine after a circumcision? – yes
§ My child is leaking through their diapers more often, is this normal – yes (the Vaseline that we instruct you to layer on the front of the diaper makes it less absorbent.
§ Etc etc!
· To help parents address these types of questions, we have tried to make accessing out medical team as seamless, secure and convenient as possible by offering a secure app-based portal offered through our electronic medical record (TELUS – CHR).
· We encourage parents to send messages and photos through this portal any time they have a concern.
· We strive to reply to all messages by the end of the day.
· Depending on the issue, we may reply to the messages with a telephone call as well. (For security and privacy reasons we will not leave a telephone voice message.)
· An overwhelming majority of the questions we receive are related to the appearance of the healing wound, and almost all these questions can be addressed by the healthcare provider after seeing images of the wound – without seeing the wound in-person.
· On the day of the clinic appointment parents receive an email inviting them to access the parent portal app. Once logged in and linked with your child’s chart, we instruct parents to :
o Please list:
§ Parent name(s):
§ Best telephone number to call:
§ Date of circumcision:
§ Child's Health Card Number (with version code):
HEALTH CARD NUMBER MUST INCLUDE VERSION CODE IF AVAILABLE
§ Please give a brief description of the concern, and if you are sending photos, please make sure to attach the images. If possible, kindly use a circle or arrow to point out the specific areas of concern in the photo:
· 1) From above
· 2) From below
· 3) From the left
· 4) From the right
· Please see the section below for a step-by-step guide on how to download, set-up and register the app.
· In some circumstances, after reviewing photos, or learning about a problem from the messages sent through the app, the health care team identifies issues that require in-person follow-up. In these cases, the family is contacted by the clinic admin to arrange the appointment.
· Similarly, some parents simply prefer an in-person appointment and aren’t comfortable sending photos. We are happy to accommodate these requests.
· The Circumcision Clinic is decentralized – meaning the team moves to different locations throughout the month.
· Follow-up appointments can be offered at a different location than the one where the circumcision took place. For urgent appointments, this might require the family to travel. For less urgent appointments, we can accommodate at the clinic location closest to you.
· Similarly, we work with a shared-care model.
o So, your appointment may be with a physician that is different than the one who performed the procedure.
· We can also address some follow-up concerns through a virtual video appointment.
· Depending on the concern, follow-up can be achieved by:
o Messaging through the secure app.
o Virtual video appointment.
o In-person clinic appointment.
· The preferred form of communication for any after-circumcision concern is through the app based secure portal. We are happy to help over the phone or by email as well. We ask parents to sign a waiver acknowledging the cybersecurity risks of communicating medical information online via email to ensure everyone is aware before transmitting sensitive information. A copy of this waiver can be found here.
· Follow-up messaging and appointments are best for non-urgent, non-life-threatening issues.
· Any life-threatening concern should prompt an urgent visit to your nearest emergency department. Life-threatening concerns are extremely rare on the day of the circumcision.
o Excessive bleeding.
§ In rare circumstances, we can discover a child has a bleeding disorder and cannot establish a clot. Though this is incredibly rare, excessive bleeding in a newborn must be urgently addressed.
o Anaphylactic or other allergic type reaction to the local-anesthetic or skin cleaning solution.
§ Any difficulty breathing, rash, lethargy should be treated urgently.
§ This is incredibly rare and at the time of writing, The Circumcision Clinic has never had a patient that has had this type of reaction.
o NOTE: There is a tendency we see for parents to associate any new behaviours / rashes / fevers / changes in bowel or urination with the circumcision. It is important to keep in mind that there can be changes in health that occur at the same time as the circumcision that might not be related. The Circumcision Clinic can offer expert advice related to the circumcision. If an issue is unrelated, we will suggest contacting a primary care provider (family doctor, pediatrician or emergency department).
· If you encounter a life-threatening issue related to the circumcision, you can contact our clinic on your way to hospital. If we are able, the clinic staff will call ahead to the emergency department to provide information to the receiving team to help them prepare ahead of the child’s arrival.